The compression syndrome of the celiac trunk was described by Harjola in 1963 as the extrinsic compression of the celiac trunk by the tendon fibers of the arcuate ligament; “Median arcuate ligament release cpt” Causing a picture of intense pain post-pandrial in epigastric, weight loss, epigastric murmur and stenosis greater than 75% in selective angiography. Since then, this syndrome has been the cause of multiple controversies related to its pathogenesis and the variability of the results obtained with the surgery.
Due to the proliferation and accessibility of more accurate and less invasive imaging techniques (Angio-Tac, Angio-NMR, echo-Doppler), the diagnosis of this syndrome can be done more precisely and lay the bases of the surgical indication with greater safety and efficacy .
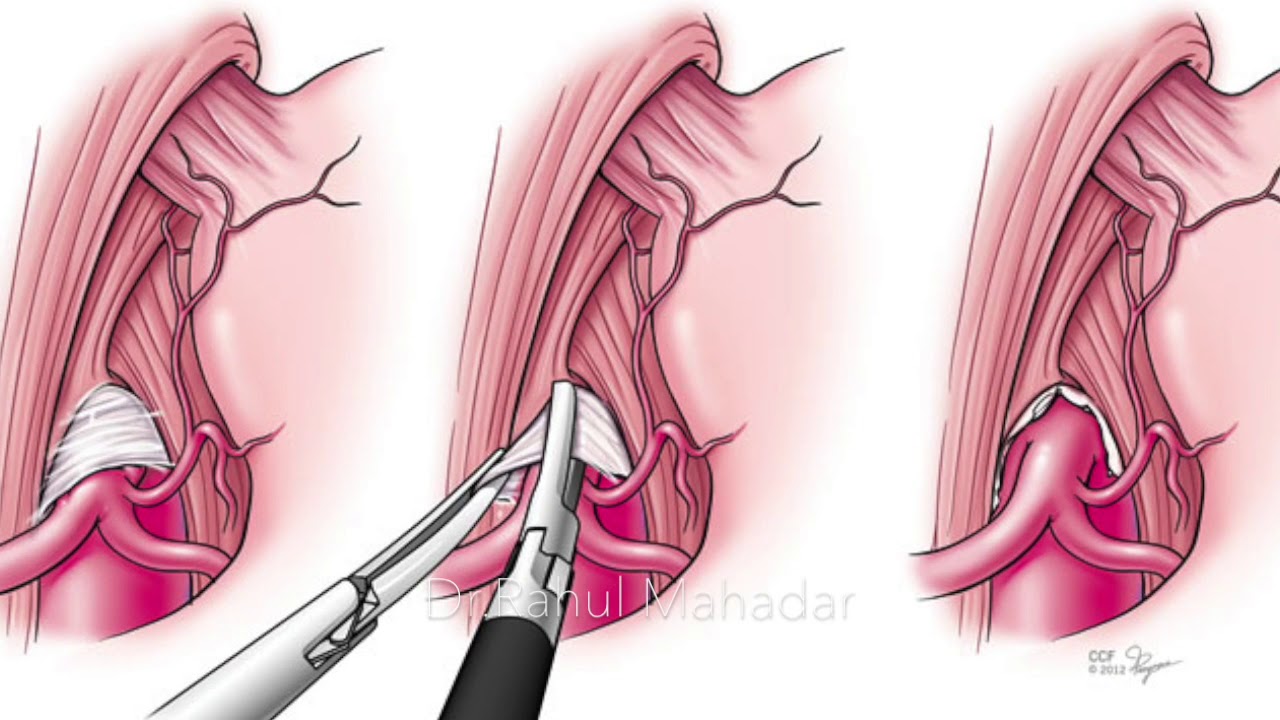
The introduction, in the year 2000, of laparoscopic techniques in the release of the Celiac trunk, along with complementary endovascular procedures, has represented a notable breakthrough in the treatment of the syndrome. Based on our personal experience, we present a critical review and therapeutic proposal of the syndrome.
The middle arcuate ligament is a fibrous arch that binds the diaphragmatic crura on each side of the aortic hiatus. On the right side the diaphragmatic Crura is originated on the anterior surface of the L1-L4 vertebral bodies and on the left side of the first two or three lumbar bodies. Crura also has insertions in the intervertebral discs and anterior longitudinal ligament.
The medium arcuate ligament, under normal conditions, passes over the aorta, at the height of the first lumbar vertebral body, superior to the origin of the celiac trunk. In a 10-24% of the population can have a more caudal route and crossing immediately above the proximal portion of the celiac trunk in a small percentage of patients with this variant can produce a hemodynamically significant compromise.
It is believed that compression is caused by an abnormally low insertion of the diaphragm or an excessively high origin of the celiac trunk in the aorta. They can also contribute to the compression of the celiac ganglion fibers. Its incidence is two per 100 000 patients with upper abdominal pain, recurrent and non-specific.
Middle arcuate ligament syndrome.
Also called extrinsic compression syndrome or Dunbar syndrome, it has an incidence of about 2/100,000 patients with recurrent upper abdominal pain. The definition of this syndrome agglutinates both a clinical and radiological diagnosis. It usually occurs in young patients, of about 20-40 years, it is more frequent in women and it is presented with a clinic of pain epigastric (can be postprandial) and weight loss. In physical exploration we can sometimes hear a murmur that varies with breathing in the middle Epigastric region. These symptoms are due to a compromise of flow caused by the arrangement of the ligament mentioned above.
Diagnosis
It can be performed by ultrasound (Fig 2) Doppler with measurements of blood velocities in the celiac trunk at the end of Insipración and exhalation. If we target peak speeds above 200 cm/sec We are facing a significant flow commitment. The appearance of the Multicut TC allows to perform angiographic studies that will provide us with valuable information on local anatomy, hemodynamic information and the presence of concomitant calcifications.
The sagittal plane (Fig 3) is optimal for visualizing the proximal portion of the celiac trunk. One fact that we should take into account is that the TC study is done in maximum inspiration that is when there is a lower compression of the ligament on the celiac trunk so we should consider doing the study in exhalation.
The criteria for distinguishing this identity from atherosclerotic stenosis of the celiac trunk are the observation of the hooked aspect due to the crease (Fig 4, 5 and 6) (especially in the proximal portion of the celiac trunk) and the indentation of the adjacent aortic rim.
Angio-MRI may be useful in children and adolescents to avoid exposure to ionizing radiation if Doppler ultrasound is inconclusive.
Treatment
The surgical treatment has been controversial because many authors have questioned that symptoms can be attributed to the isolated narrowing of the celiac trunk as there is a significant percentage of patients showing the anomaly and lack of symptoms. The treatment consists of the division of the median arcuate ligament by laparoscopy with the release of celiac trunk and the realization of revascularization procedure if it has occurred. This treatment is more likely to succeed in 40-60 patients with postprandial pain, post-stenotic dilatation, and collateral vessels.
Conclusions:
Although there is no consensus on whether the middle arcuate ligament syndrome is a real entity, the improvement of many of the patients after proper treatment forces the radiologist to have this diagnosis in mind when dealing with cases of abdominal pain without apparent cause.